Table of Contents
-
Understanding Pet Dental Anatomy
1. Understanding Pet Dental Anatomy
More Than Just Teeth: A Complex Oral System
Pet dental health encompasses the entire oral cavity ecosystem, including teeth, gums, tongue, and supporting structures. This system functions not only for food acquisition and processing but also plays crucial roles in temperature regulation, social interaction, and defensive behaviors. Understanding this complexity helps American pet owners appreciate why comprehensive dental care extends beyond occasional tooth brushing.
The domestic canine possesses 42 permanent teeth designed for grasping, tearing, and crushing, while domestic cats have 30 permanent teeth specialized for precision killing and meat shredding. These dental formulas reflect evolutionary adaptations that remain relevant even in modern pet diets.
Periodontal Structures and Their Functions
-
Enamel: The hardest substance in the body, protecting teeth from wear and decay
-
Dentin: Softer tissue beneath enamel that forms the tooth’s main structure
-
Pulp: Living core containing nerves and blood vessels
-
Periodontal Ligament: Collagen fibers anchoring teeth to jaw bones
-
Gingiva: Mucosal tissue providing protective barrier and support
Q: Why do pets rarely get cavities compared to humans?
A: Pet teeth have different shapes with wider grooves, diets typically contain less refined sugar, and their oral bacteria differ significantly from humans. However, pets face greater risk from periodontal disease, which affects over 80% of dogs and 70% of cats by age three.

2. The Science of Oral Health
The Plaque-to-Tartar Transformation
Oral health deterioration follows a predictable biological sequence. Within hours after eating, oral bacteria form an invisible biofilm called plaque on tooth surfaces. If not removed within 24-48 hours, minerals in saliva calcify this plaque into dental calculus (tartar), which creates a rough surface attracting more plaque accumulation.
This cycle initiates an inflammatory response in the gums (gingivitis), which can progress to destruction of the tooth-supporting structures (periodontitis). The constant bacterial presence in the mouth allows toxins to enter the bloodstream, potentially affecting distant organs including the heart, liver, and kidneys.
Species-Specific Oral Health Considerations
Understanding fundamental differences between canine and feline oral health challenges informs appropriate care strategies:
Canine Oral Health Characteristics
-
Varying susceptibility by breed size and skull shape
-
Natural chewing instincts providing some mechanical cleaning
-
Common developmental issues like retained deciduous teeth
-
Frequent periodontal pocket formation, especially in small breeds
Feline Oral Health Challenges
-
Greater susceptibility to tooth resorption lesions
-
Higher incidence of chronic gingivostomatitis
-
Increased sensitivity to dental procedures
-
Subtle pain expression complicating early problem detection
Q: Can dental problems really affect my pet’s overall health?
A: Absolutely. The constant bacterial presence in periodontal disease allows toxins to enter the bloodstream, potentially affecting distant organs. Research shows pets with good dental health typically live 15-20% longer than those with chronic dental issues, highlighting the systemic importance of oral care.
3. Complete Dental Care Protocol
The Four-Phase Dental Health Framework
Phase 1: Professional Assessment and Baseline Establishment
Begin with a comprehensive veterinary oral examination to establish your pet’s dental health status and identify any existing issues requiring intervention. This assessment should include:
-
Tooth-by-tooth evaluation for mobility, fractures, or resorptive lesions
-
Periodontal probing to measure pocket depths around each tooth
-
Dental charting documenting all findings for future comparison
-
Discussion of appropriate timing for professional cleaning if indicated
Phase 2: Home Care Implementation
Implement consistent daily care practices tailored to your pet’s specific needs and tolerance levels:
Acclimation Protocol
-
Introduce dental tools gradually without expectation of immediate success
-
Associate all dental care with positive experiences through reward-based training
-
Progress systematically from mouth touching to brief tooth exposure to actual cleaning
-
Respect your pet’s comfort limits while gently expanding tolerance
Brushing Technique Mastery
-
Use appropriate pet-specific cleaning tools with soft bristles
-
Focus on the outer tooth surfaces where plaque accumulates most heavily
-
Employ gentle circular motions at the gum line where plaque initiates
-
Target 30-60 seconds total brushing time, gradually increasing as tolerance improves
Phase 3: Professional Intervention Planning
Schedule professional dental cleanings based on your veterinarian’s recommendation, considering your pet’s:
-
Individual susceptibility to periodontal disease
-
Effectiveness of home care routine
-
Age and overall health status
-
Specific breed predispositions to dental issues
Phase 4: Ongoing Monitoring and Maintenance
Establish regular assessment practices to detect changes in oral health status:
-
Weekly visual inspections of gums and teeth
-
Monthly breath odor evaluation
-
Quarterly veterinary oral assessments during routine visits
-
Annual professional cleanings for most adult pets
Effective Alternative Cleaning Methods
For pets who cannot tolerate tooth brushing, several evidence-supported alternatives exist:
-
Dental wipes for mechanical plaque removal
-
Approved dental diets with mechanical or chemical cleaning action
-
Veterinary-recommended water additives reducing bacterial load
-
Appropriate dental chews selected for safety and efficacy
Q: How can I tell if my pet has dental pain since they hide discomfort so well?
A: Watch for subtle signs including decreased interest in hard food or toys, unusual drooling, pawing at the mouth, reluctance to have head touched, personality changes, or unexplained irritability. Many pets continue eating despite significant dental pain, making behavioral observation crucial for early detection.
4. Advanced Prevention Strategies
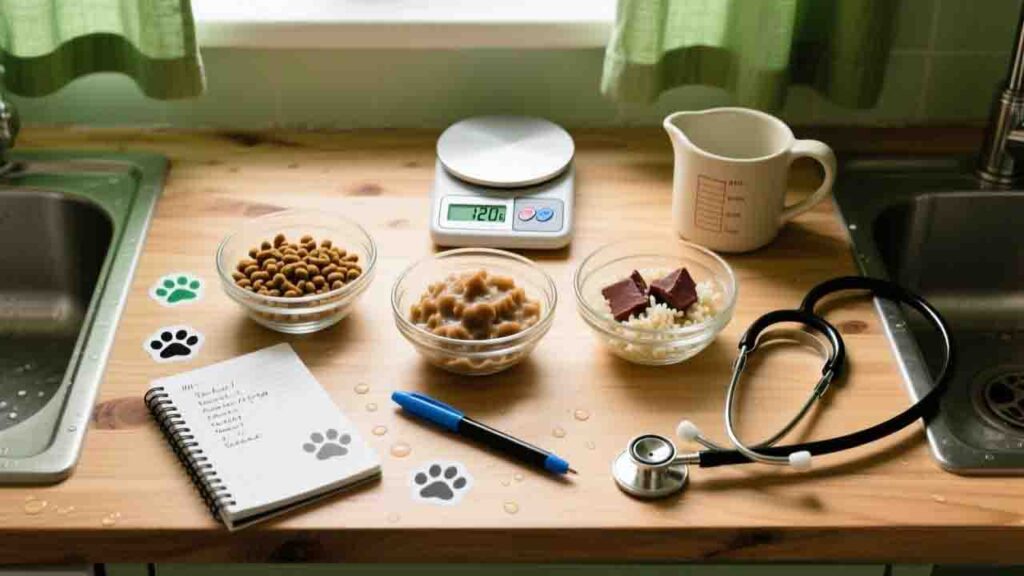
Nutritional Support for Oral Health
Diet plays a significant role in dental disease prevention through several mechanisms:
Mechanical Cleaning Action
Select foods with appropriate texture and structure that provide natural cleaning through chewing action. These diets work through abrasion against tooth surfaces and stimulation of saliva production, which helps neutralize acids and wash away food particles.
Chemical Plaque Reduction
Some specially formulated diets contain polyphosphates that bind calcium in saliva, reducing tartar formation. These ingredients work systemically after being released during eating and mixing with saliva throughout the mouth.
Environmental Enrichment for Oral Health
Incorporate dental-friendly activities into your pet’s routine:
Appropriate Chewing Opportunities
Provide safe, veterinary-recommended chewing items that satisfy natural instincts while supporting dental health. The mechanical action of chewing helps reduce plaque accumulation, particularly on rear teeth where brushing is most challenging.
Interactive Dental Toys
Utilize toys designed to support oral health through approved mechanical action. These products should be selected based on safety, effectiveness, and appropriateness for your individual pet’s chewing style and dental status.
Comprehensive Health Management
Address underlying factors that influence oral health:
Weight Management
Maintain ideal body condition, as obesity correlates with increased periodontal disease risk and complicates anesthesia for dental procedures when needed.
Systemic Health Monitoring
Manage conditions like diabetes and kidney disease that significantly impact oral health. Conversely, maintain excellent oral health to reduce systemic inflammatory burden on these organs.
Q: Are anesthetic dental cleanings safe for senior pets?
A: Modern anesthetic protocols make dental procedures remarkably safe, even for older pets. Comprehensive pre-anesthetic testing, individualized drug selection, and advanced monitoring during anesthesia minimize risks significantly. The dangers of untreated dental disease typically far exceed anesthetic risks, as chronic oral infection creates constant systemic stress.
5. Common American Pet Owner Misconceptions
The “Hard Food Cleans Teeth” Fallacy
Many owners believe dry food automatically provides adequate dental cleaning. While some specially formulated dental diets have demonstrated effectiveness, regular dry food provides minimal mechanical cleaning action. The carbohydrate content of many dry foods may actually contribute to plaque formation, making this one of the most persistent and dangerous dental care misconceptions.
The “Bad Breath is Normal” Misconception
Accepting unpleasant pet breath as normal prevents early detection of serious dental issues. Unlike humans where certain foods cause temporary odor, persistent bad breath in pets typically indicates bacterial activity associated with periodontal disease. Offensive odor warrants veterinary assessment rather than resignation or masking attempts.
The “No Visible Problems Means Healthy Mouth” Error
Assuming absence of obvious issues indicates good oral health represents a significant detection barrier. Periodontal disease begins below the gum line where owners cannot see it, and pets instinctively hide dental pain. Regular professional assessments are necessary to identify developing issues before they become advanced problems.
The “Anesthesia-Free Cleanings are Safer” Misconception
Non-anesthetic dental cleanings create a false sense of security while addressing only the visible crown surfaces. These procedures cannot access subgingival areas where disease originates, cannot perform necessary probing and charting, and may cause significant stress while delivering incomplete care.
The “Dental Health is Cosmetic” Minimization
Considering dental care as merely aesthetic overlooks its profound impact on overall health. Chronic oral inflammation affects distant organs, dental pain diminishes quality of life, and oral infections can become systemic. Dental health represents a medical necessity rather than a cosmetic luxury.
Q: My pet hates tooth brushing – should I just give up?
A: Absolutely not. Many alternatives exist, and success often requires finding the right approach for your individual pet. Consider different tools (finger brushes, dental wipes), various rewards, alternative cleaning methods, and professional guidance. Even imperfect dental care provides significant benefits compared to complete neglect. Consistency and patience typically yield gradual improvement in tolerance over weeks or months.